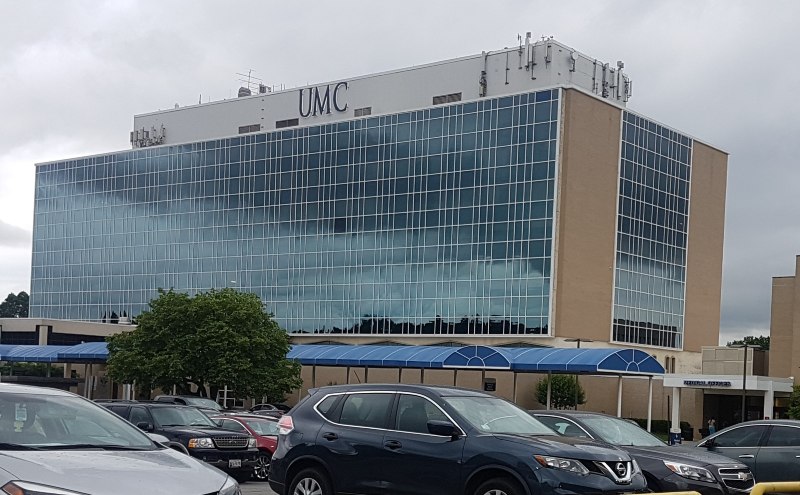
The District’s only general hospital east of the Anacostia River faces major spending cuts — a decision both employees and patients say feels like a betrayal.
United Medical Center (UMC) will likely undergo significant spending reductions starting Oct. 1, owing to a new fiscal oversight board established by the D.C. Council in May. Both staff and patient services are expected to be hit as the oversight board copes with the D.C. Council’s new subsidy limit — just $15 million from the city to cover the hospital’s more than $40 million annual deficit. Details about the cuts will be released in July.
Lawmakers in favor of the board and subsidy cap explained their decision is intended to limit city spending while a new replacement hospital is constructed nearby. That hospital, however, won’t be completed for several years. To residents who rely on UMC’s services, these cuts are the latest in a long history of neglect from city officials.
UMC, now a nonprofit operation owned by the D.C. government, has long struggled financially. The facility has undergone multiple bankruptcies and owners since it began operating in 1966, but the exact cause of its struggles today is a point of contention.
According to D.C. Deputy Mayor for Health and Human Services Wayne Turnage, the story is one of overstaffing and years of decline in patient volume. UMC’s nurses, however, report feeling severely understaffed, and attribute the hospital’s finances to mismanagement and a lack of support.
“The hospital runs on average about 70 patients a day, and when it varies it tends to vary down,” Turnage said during a D.C. Council hearing in May. He described a 10-to-1 staff-to-patient ratio at UMC, including both nurses and other non-clinical staff. “If you look at their staff and compare it to the standards suggested by the American Hospital Association, they are 45% overstaffed.”
The American Hospital Association (AHA) has no publicly available standards on typical hospital staffing ratios and could not be reached before publication, but the organization does have a history of opposing nurse staffing ratio mandates. In an online policy declaration, the group describes mandated staffing ratios as “a static and ineffective tool that cannot guarantee a safe health care environment or quality level to achieve optimum patient outcomes.”
Wala Blegay, staff attorney and labor specialist for the District of Columbia Nurses Association, contests Turnage’s characterization. According to her, Turnage is undercounting UMC’s patient load by only including in-patients — those admitted to the hospital for treatment after being processed through the emergency room or behavioral health unit.

“If you are in critical condition and you need to go to the [Intensive Care Unit], but the ICU only has room for four to five people, they can’t transfer you to ICU so they might have to transfer you out of the hospital or keep you in the [Emergency Room],” Blegay said. “Technically you’re not in-patient because you’re in the ER, even if you’re in the ER for a long time, because the ICU can’t take you. So the reason why the actual hospital has a low [patient] number is due to the limited services, not due to people not coming to the hospital.”
Because the hospital does not offer specialty care services like cancer treatment, many UMC-processed patients are transferred to other D.C. hospitals rather than admitted. On top of this, most of UMC’s patients are on Medicaid and Medicare, thereby generating less revenue for the hospital when billed. These conditions together have left the hospital in an untenable financial position, according to Blegay.
“If you take surgery, cancer, all of these things out of the hospital, then you have a hospital that really only gives general care. General care, even emergency care, is not enough to pull any hospital through,” Blegay said.
Turnage, in a comment to Street Sense Media, defended his measurement of UMC’s patient volume. It is “one standard used by the industry,” he wrote. Additionally, Turnage said that while his office monitored UMC’s daily in-patient census more closely than others, patient volume metrics across the board showed similar declines.
“Almost without exception, the trend for those metrics at UMC that drive revenue — admissions, patient days, ER visits, and inpatient surgeries — are either negative, or the total volume of the activity is much lower than what you would expect to see at a robust acute care hospital,” Turnage wrote.
According to data Turnage’s office provided to Street Sense Media, emergency room visits are down 20% compared to the previous year and the number of days patients spent in the hospital are less than half of what they were this time last year. Though these statistics were impacted by COVID-19, the negative trends at UMC also predate the pandemic.
Roberta LeNoir, an emergency room nurse and the collective bargaining unit president in the Nurses Association, pushed back against the notion that UMC is overstaffed. She described a hospital that repeatedly struggles to keep up with its current patient volume — precisely because it lacks necessary funding from the city.

“We have people coming from all over, and we’re doing the best we can with what little resources we have. We’re being strangled from the top financially by cutting our services, and we’re being just beaten to death from the bottom by the amount of patients that come in. And it’s awful because even though we’re seeing the patients, we’re not getting the revenue because we got to transfer them out,” LeNoir said. “It makes no sense. How are we to make money if we got to transfer everybody out?”
LeNoir recounted how inadequate staffing forced her and her colleagues to balance patient care with a myriad of other responsibilities — even basic custodial duties.
“We’re past skeleton staffing, we’re down to a bone,” LeNoir said. “When gunshot wounds run in or stabbings run in, they routinely drip blood from the lobby or ambulance bay into the [Emergency Department]. If they don’t have enough staff, you have to decide whether you’re going to let the blood stay there or get it up, and you’re going to get it up because you don’t want the clients walking in blood.”
According to LeNoir, the situation has gotten worse over time as UMC’s declining financial situation has forced repeated rounds of permanent staffing cuts, known as reductions in force (RIF). “That’s normal,” LeNoir said, noting she’s been through several such reductions.“When they have these RIFs, they do not rehire the people, they don’t refill the positions. We have to make do with what we have.”

This understaffing has had consequences for patients who visit UMC for care. The Washington Post featured one neighbor of the hospital who said he travels across town to the George Washington University Hospital when in need of care. But for many residents in Wards 7 and 8, UMC is their only option.
[Read more: With limited access to hospital resources in wards 7 and 8, local clinics are bridging the gap in health care]
“We still have all of these people coming in [to UMC] — people that are looking for doctors to deliver their babies — and the reason why they’re coming there is because most of our people do not have the funds to travel up Northwest,” said Christopher Hawthorne, a community leader and former Ward 8 ANC commissioner. “And that’s one of the sad parts. For most of these operations that they need, they simply do not have the time to be traveling such a far way.”
Residents of wards 7 and 8 suffer from a disproportionately high number of negative health outcomes compared with the rest of the District. African American residents, specifically, live with increased risk for hypertension, diabetes, obesity, and other conditions, according to a 2016 study by Georgetown University.
As a result, COVID-19 mortality rates in UMC’s intensive care unit are far above the national average — 47% of admitted coronavirus patients have died to date, according to an April report from UMC’s hospital board. That same report noted that approximately 9% of UMC patients left without seeing a provider in March — a slight decline from the previous month, but still more than four times the national average.
UMC’s nurses have been calling attention to the hospital’s mismanagement for years. Back in 2017, after the hospital permanently shuttered its obstetrics ward due to reported mishandlings of pregnant patients, the nurses took a vote of no confidence against the consulting firm that ran the hospital. At the time, UMC’s top doctor accused the firm, Veritas, of “disregard[ing] patient care and committ[ing] malfeasance in its effort to increase patient volume.” This led the city to switch contractors in 2018 from Veritas to UMC’s current operator, Mazars.
[Read more: Health care professionals urge DC to build a “full-service” hospital east of the Anacostia River]
D.C. Chief Financial Officer Jeffrey DeWitt called the hospital “functionally” bankrupt in 2018, as Mazars was onboarded. According to Turnage, UMC revenues since then have declined by 10% to $100 million, while expenses have only declined by 4% to $142 million in the same period. Moreover, Turnage expects that $42 million dollar deficit to grow in the next year. “My guess is, given the decline in patient activity and the lingering effects of the pandemic, that [revenue] may drop below $100 million in 2022,” Turnage said at the May hearing.
These incidents have motivated city officials to invest in a new facility meant to replace UMC by 2024. As part of a 2019 plan to speed up the replacement hospital’s construction at St. Elizabeths East Campus in Ward 8, the Council capped the amount of subsidies UMC could receive annually; any funding above the Council’s designated $15 million subsidy threshold would trigger the fiscal control board to rein in spending.
The Council’s subsidy limit became relevant last month as Mayor Bowser allocated an additional $25 million to the hospital in order to cover payroll and other expenses for the remainder of this fiscal year. Ward 7 Councilmember Vincent Gray introduced emergency legislation in order to raise the subsidy limitation from $15 million to $40 million, which would have avoided the fiscal oversight board and the service cuts that will accompany it. But the bid failed by two votes. UMC received the $25 million to stay afloat through Sept. 30, but will now have its budget dramatically downsized by the oversight board going forward. The fiscal control board is expected to stay in place until UMC’s replacement hospital opens.
Though the city is funding construction, the new hospital at St. Elizabeths will be privately operated by United Health Services, the same company that operates George Washington University Hospital. This also means UMC’s closure will leave D.C. without any public hospitals. While private hospitals traditionally offer more personalized care and shorter wait times, they are also smaller and more cost-prohibitive for patients — St. Elizabeths is planned to have fewer beds than UMC, but will offer more specialty care services.
The emergency bill’s failure came as a frustrating surprise to the hospital’s staff, including LeNoir. She and Blegay testified before the Committee on Health — chaired by Gray — in the aftermath, commenting on June 7 that the Council’s actions felt contradictory to their constituents’ values. “It is difficult for us at UMC to believe that Black lives of residents in wards 7 and 8 really matter,” LeNoir said at the time.
D.C. Council Chairman Phil Mendelson, who voted against the emergency bill, blamed UMC’s administrators for the hospital’s continual financial woes. “The hospital has to account for what they say and control their spending. There seems to be an expectation that they don’t have any budgetary constraints,” he wrote in a statement to Street Sense Media.
The since-appointed fiscal control board is expected to deliver its reduced spending plan to the D.C. Council next month. Angell Jacobs, the board’s chair and former D.C. Deputy Chief Financial Officer, testified during a June 7 hearing that the board will “strive to minimize the impact to those delivering direct services to our patients.”
In addition to Jacobs and Turnage, the fiscal control board’s members include former city administrator Robert Bobb, vice chair of UMC’s board of trustees Dr. Malika Fair, D.C. Nurses Association representative Donita Reid-Jackson, and Service Employees International Union representative Girume Ashenafi. The hospital’s interim CEO, Marcela Maamari, and its chief medical officer, Dr. William Strudwick, are also non-voting members of the board.
Though the 2019 legislation first establishing the oversight board required the mayor to specifically appoint a Ward 8 resident as a member, the D.C. Council removed that stipulation last month. Lawmakers changed the language so that the appointee could be from either Ward 7 or 8 — a requirement Dr. Fair, a Ward 7 resident, meets. The last-minute change discouraged Hawthorne, who says he feels unrepresented in the decisions surrounding his community’s hospital. “At this point in time, we have no one to advocate for the community that’s serving on that board,” Hawthorne said.
His frustrations, however, stretch beyond just the impending spending cuts. For him and his neighbors, the fiscal control board is the latest in a pattern of city officials breaching the trust of their most vulnerable residents.
[Read more: The fate of United Medical Center remains unsettling to many residents of wards 7 and 8]
“Our District leaders are hypocrites to their fiduciary duties,” Hawthorne said. “We still pay taxes. We should have a hospital in our area. And if we wanted to have two — UMC and the new hospital — to handle the volume of people, we should very well have it. But we’re not allowed to have those things.”
Until the new spending plan is released in July, nurses like LeNoir can only wait and hope to weather the storm to come. It’s not the first time they’ve had to.
“I would like it to be known that the same staff that works at UMC works at other area hospitals,” LeNoir said. “We are trained. We save lives everyday. We do the very best we can. And we have no control over the management companies that have been brought in that have raped that hospital time and time again.”
“We never get to vote on who comes in or what they do when they get there. But we have to carry the brunt of ‘Oh well, that’s UMC.’”